What Is Lupus?
Chances are you have heard about lupus over the past year, whether that be on the news where a celebrity was newly diagnosed with it, or you personally know someone afflicted by the disease.
But do you truly know what lupus is? To put it simply, lupus is an autoimmune disorder, one that results in chronic, excessive all over inflammation in the body. Not surprisingly, many persons afflicted by lupus are prone to developing organ damage, or developing other inflammatory disorders such as psoriasis or irritable bowel syndrome.
In some persons it can be severe and life-threatening, even though most of the persons that develop the disorder are lucky to only experience milder symptoms.
Types Of Lupus
Not everyone that develops lupus will experience the same symptoms. In actuality, there are four different types of lupus that one can develop. These are:
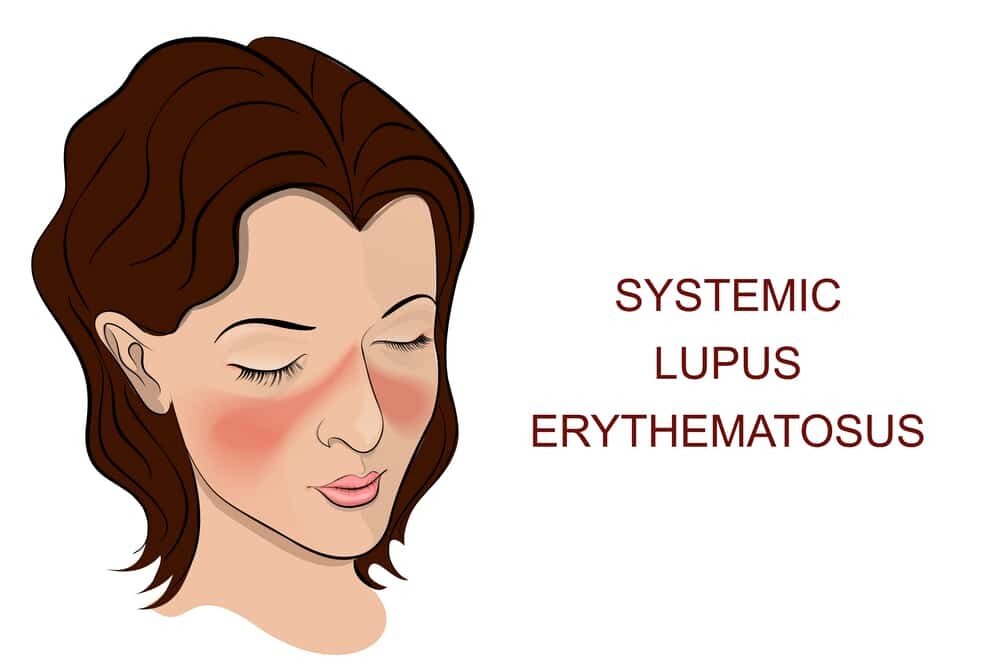
Systemic Lupus Erythematosus (SLE)
This is by far the most common type of lupus, and the most serious. Most of new cases of lupus diagnosed are of this variety, causing excessive inflammation to occur in any part of the body.
Systemic lupus erythematosus can follow an unpredictable pattern of active flare-ups, followed by remission when no symptoms are obvious. However, flare-ups are generally more severe and can greatly contribute to damage of important organs such as the kidneys, liver, skin, hearts, lungs or even the blood, which can be considered an active transport organ.
It is very important for you to keep an eye on symptoms, as it can get worse very quickly.
Discoid Or Cutaneous Lupus
This type of lupus affects primarily the skin, and may resemble eczema, resulting in development of inflammatory patches, primarily on the face, scalp and neck. Even though the symptoms of this type of lupus are primarily reserved for skin, approximately 10% of the persons with discoid lupus will develop systemic lupus over their lifetime.
Drug-Induced Lupus
This is not true lupus per se, but rather the induction of lupus like symptoms following the usage of specific medications. Symptoms usually disappear upon cessation of the medication, which is good, but may lead to false systemic lupus diagnosis as a result of indicators that may persist years afterwards.
Anti-nuclear antibody tests, commonly used to diagnose new cases of lupus, may still indicates positive findings for many years, so that needs to be put into perspective to rule out true lupus.
Neonatal Lupus
Rarely, a baby born to a mother with systemic lupus will develop lupus himself, resulting in severe skin rashes, anemia or other associated organ problems. Luckily, this type of lupus seems to resolve within six months of birth, but is not without its own set of risks.
For instance, babies born with neonatal lupus are at a significantly higher risk of cardiovascular problems, with some even being born with a major heart defect.
Symptoms Of Lupus
Even though the exact lupus symptoms very based on the type diagnosed, in general one or more of these symptoms will be present, especially in systemic lupus patients.
- Chronic fatigue or lethargy
- Hair loss as a result of inflammatory damage to the scalp
- Arthralgia, especially early onset arthritis
- Chronic low-grade fever that does not resolve with commonly used antipyretic medications
- Suppressed appetite
- Muscle aches and pain
- Mucous membranes that easily damage – canker sores and bleeding is very common in the mouth
- A diverse facial rash resembling the shape of a butterfly (a butterfly rash)
- Abnormal sensitivity to sunlight, triggering rashes on the skin (photosensitivity)
- Pain in the chest as a result of inflammation to the lining around the heart or lungs
- Poor extremity blood circulation, especially when exposed to cold
- Organ scarring – complications frequently occur when organ specific tissue is scarred, eventually leading to organ failure (for example, liver cirrhosis)
- Anemia and poor blood clotting as a result of impaired platelet formation
- Seizures, personality changes, or even death due to changes in the brain caused by excessive inflammation
- Heart disease as a result of blood vessel inflammation and increased risk of cholesterol deposition
Possible Causes Of Lupus/ Risk Factors
Even though lupus may develop spontaneously in the absence of any triggers, there are a few factors that increase one’s risk. These include:
Environmental Factors
Cigarette smoking, chronic heavy stress burden and toxins such as asbestos or silica dust can all contribute to the development of lupus.
Hereditary Links
Lupus shares a strong genetic link that increases your risk exponentially if a first-degree relative also has lupus.
Specific Hormones
Premenopausal women are more likely to develop lupus, as higher estrogen levels could contribute to the development of lupus.
Prescription Medication
Long-term use of certain medications such as hydralazine, a popular blood pressure lowering medication, or quinidine, used for arthritis treatment or malaria, all contribute significantly to the development of drug-induced lupus. Switching to a suitable alternative is the best way to go to reduce your risk.
Infections
Certain viral infections raise of you developing lupus, owing to changes they cause at the genetic level. These include the Epstein-Barr virus, viruses that cause hepatitis, and cytomegalovirus.
Ethnicity
Ethnic groups except Caucasians have an increased risk of developing lupus. If you are of the African, Asian, Pacific Islander, Hispanic or Native American ethnicities, your risk is higher.
Age
Lupus is more likely to occur in persons between the ages of 15 to 45.
In addition to these, idiosyncratic lupus is also commonly reported, in the absence of these risk factors.
Treatment Of Lupus
There is currently no cure for lupus, even though treatment modalities can significantly improve quality of life, and enable persons with lupus to live as close to normal as possible. It is estimated that between 80 to 90% of persons diagnosed with lupus will be capable of living full, normal lives with good management techniques.
Commonly used treatment modalities include
NSAID Painkillers
Most of these are over the counter remedies for treatment of pain and inflammation, lending themselves perfectly to management of muscle and joint issues. However, they do come with their own set of inherent risks, so be sure to discuss them with your physician.
Corticosteroids
Corticosteroids are some of the most potent anti-inflammatory compounds used in the management of lupus, commonly used ones being prednisone, or topical applications such as betamethasone.
Pro-Hormones
Including DHEA, these help to convert into male hormones such as DHT, which supports hair growth in persons not predisposed to male pattern baldness (useful for cutaneous lupus).
Immuno-Suppressants
One of the mainstays of treatment, these reduce activity of your immune system so that less autoimmune activity occurs. These carry the risk of increasing your susceptibility to infections greatly, so be sure to keep in mind all the considerations your physician advises you.
Lifestyle Modifications
Your physician may also advise you to change your lifestyle in certain regards, such as avoiding unnecessary sun exposure, eating a more anti-inflammatory diet, quitting smoking or drinking, and using supplements that promote your overall health and well-being.
Conclusion
Owing to the fact that the majority of persons reading this will likely have systemic lupus erythematosus (SLE), your primary objective should be to preserve your health over the long term.
A large number of persons will be able to live a normal and fulfilling life given that short-term indulgences are restricted (think of sport drinking and smoking), a healthy diet is consumed, and you regularly follow up with your physician.


